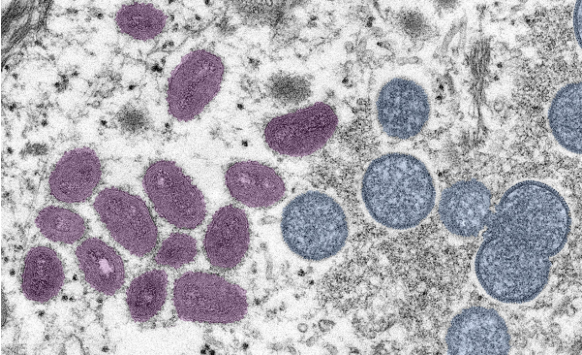
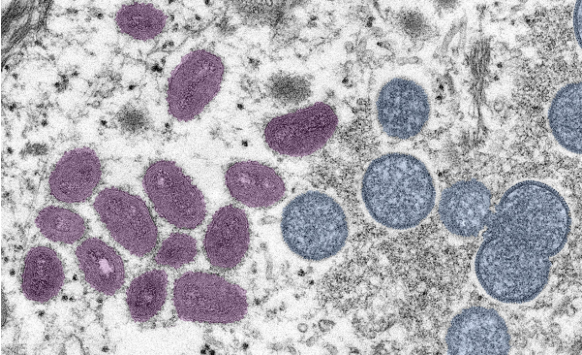
Electron microscope image of the Monkeypox virus. Image: CDC
Investigating Monkeypox: An Explainer and Resource Tipsheet
Read this article in
Human monkeypox, an infectious disease caused by the monkeypox virus, was first discovered 70 years ago. The virus has been present in parts of Central and West Africa, as a result of animal-to-human and human-to-human transmission.
In recent years, a handful of researchers who study the virus tried to notify the international community about a brewing problem, but their reports went mostly unnoticed until an outbreak in the United Kingdom this May.
The outbreak has now spread to more than 90 countries.
“This virus has been spreading in marginalized and vulnerable populations [in Africa] for decades, and we’ve done nothing about it,” Dr. Anne Rimoin, a University of California, Los Angeles epidemiology professor, told NPR in July.
In a July 2022 comment article in Nature Reviews Microbiology, two researchers at American University of Nigeria in Yola wrote that the current outbreak of monkeypox in countries where the virus transmission hasn’t been endemic is likely “a consequence of the failure to curtail the spread of the disease in endemic regions of Africa despite decades of constant outbreaks.”
A study about monkeypox infections between April and June this year, published in the New England Journal of Medicine (NEJM), notes that although “monkeypox virus has circulated for decades in regions where it has traditionally been endemic, research into monkeypox has been neglected and underfunded.”
As of August 23, more than 41,000 monkeypox cases and at least a dozen deaths have been reported in 94 countries, 87 of which have not had a monkeypox outbreak before. The US has reported more than 14,100 cases and no deaths, according to the US Centers for Disease Control and Prevention (CDC).
On July 23, nearly two months after the UK reported its first monkeypox case, the World Health Organization (WHO) declared monkeypox a global health emergency — also called Public Health Emergency of International Concern, or PHEIC — which signals the need of an international response to ramp up available testing, medications and vaccines.
The first monkeypox case in the US was identified on May 18 in Massachusetts. On Aug. 4, the US declared a public health emergency, which allows the administration to use federal funds to respond to the outbreak.
To help journalists with their continued reporting of the outbreak, we’ve gathered several key facts and peer-reviewed studies on monkeypox. As you will see in the collection of studies below, scientists have been sounding the alarm for years leading up to the current outbreak, calling for more research and better surveillance. We’ll update this piece regularly as new information and research comes to light.
First, let’s begin with the basics.
A brief history: Monkeypox was first discovered in 1958 in monkeys that were shipped from Singapore to Copenhagen, Denmark, for polio vaccine research. At the time, researchers called it a pox-like disease. Despite being named “monkeypox” in the following years, the source of the disease remains unknown, according to the CDC. African rodents and non-human primates like monkeys might harbor the virus and infect people. The first case of human monkeypox was found in 1970 in the Democratic Republic of Congo in a nine-month-old boy.
The virus: The monkeypox virus is a member of Orthopoxvirus genus, from the family Poxviridae, and is related to smallpox and cowpox viruses. Monkeypox is less contagious than smallpox and causes less severe illness. (Smallpox was declared eradicated worldwide in 1980. Chickenpox is from a different virus family called Herpesviridae.)
History of outbreaks in the US: The first monkeypox outbreak outside of Africa was documented in the US in 2003. Eighty-one cases in Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin were reported during the outbreak. The outbreak was linked to a shipment of animals from Ghana. In 2021, one instance of the infection was documented in a US resident who had returned from Nigeria.
Transmission: Researchers still don’t know in which host the monkeypox virus naturally lives and reproduces, but several animal species are susceptible to the virus, including rope and tree squirrels, Gambian pouched rats, rodents named dormice and non-human primates (monkeys).
Animal-to-human transmission of the virus — also called zoonotic transmission — can occur from direct contact with the blood, bodily fluids, or lesions of infected animals. Human-to-human transmission can result from close contact with respiratory secretions like droplets, skin lesions of an infected person or objects like bedsheets used by someone who has monkeypox. Transmission can also occur via placenta from mother to fetus or during birth.
Transmission via respiratory droplets usually requires prolonged face-to-face contact. This puts health workers, household members, and other close contacts of active cases at greater risk.
So far, data suggests that gay men, bisexual men and men who have sex with men make up the majority of monkeypox cases in the outbreaks in the US and other countries. But anyone, regardless of sexual orientation or gender identity, who has been in close, personal contact with someone who has monkeypox is at risk, according to the CDC.
Symptoms: The symptoms of the current monkeypox outbreak include a rash that could be on or near the genitals or anus. It can also be on hands, feet, mouth, face, and chest. Other symptoms are fever, chills, exhaustion, muscle aches, headaches, and sore throat. The illness lasts between two to four weeks.
Death rate: Over the decades, the death rate from monkeypox infection has ranged from zero to 11%, but researchers estimate the death rate from the current outbreak is about 0.03%.
Treatment: There is no specific treatment for monkeypox, but antivirals such as tecovirimat (TPOXX) may be recommended for people who are more likely to get severely ill, like patients with weak immune systems, according to the CDC.
Vaccines: Vaccination against smallpox has been shown to be 85% effective in preventing monkeypox. Jynneos, manufactured by Bavarian Nordic A/S, is currently the only FDA-licensed vaccine in the US to prevent the infection. (Jynneos is known as Imvanex in Europe, and Imvamune in Canada.) The vaccine was first approved in 2019 in the US for the prevention of smallpox and monkeypox. People exposed to the virus can also get vaccinated. The CDC recommends vaccination within four days from the date of exposure. ACAM2000 is another vaccine that’s FDA-licensed to prevent smallpox, but it is associated with higher risk of adverse reactions compared with Jynneos. For more on monkeypox vaccine availability, read the August 17 monkeypox outbreak alert by Johns Hopkins University’s Center for Health Security. A Vox piece by Keren Landman is also a good explainer about why ACAM2000 isn’t currently used. And Monkeypox Vaccine 101 by epidemiologist Katelyn Jetelina is a good overview.
A July 2022 report by the Kaiser Family Foundation explores at the local level whether jurisdictions are requesting the vaccines allocated to them. It finds that jurisdiction request rates for Jynneos vary widely. While most jurisdictions have requested their full supply of the vaccine, some have requested a percentage of their allocation. Ten states — Washington, Missouri, Kansas, Georgia, Nevada, Montana, South Dakota, Oklahoma, Kentucky, and Arkansas — had requested 50% or less of their share when the report was published.
Renaming the virus: The World Health Organization is in the process of renaming the virus, after calls by many groups, including a letter signed by 22 scientists in June.
“The prevailing perception in the international media and scientific literature is that MPXV [monkeypox virus] is endemic in people in some African countries,” the group writes. “However, it is well established that nearly all MPXV outbreaks in Africa prior to the 2022 outbreak, have been the result of spillover from animals to humans and only rarely have there been reports of sustained human-to-human transmissions. In the context of the current global outbreak, continued reference to, and nomenclature of this virus being African is not only inaccurate but is also discriminatory and stigmatizing.”
WHO has already renamed two variants of the virus. The former Congo Basin variant was renamed Clade one (I) and the West African variant is now Clade two (II). Clade is a scientific term for a group of organisms that have evolved from a common ancestor.
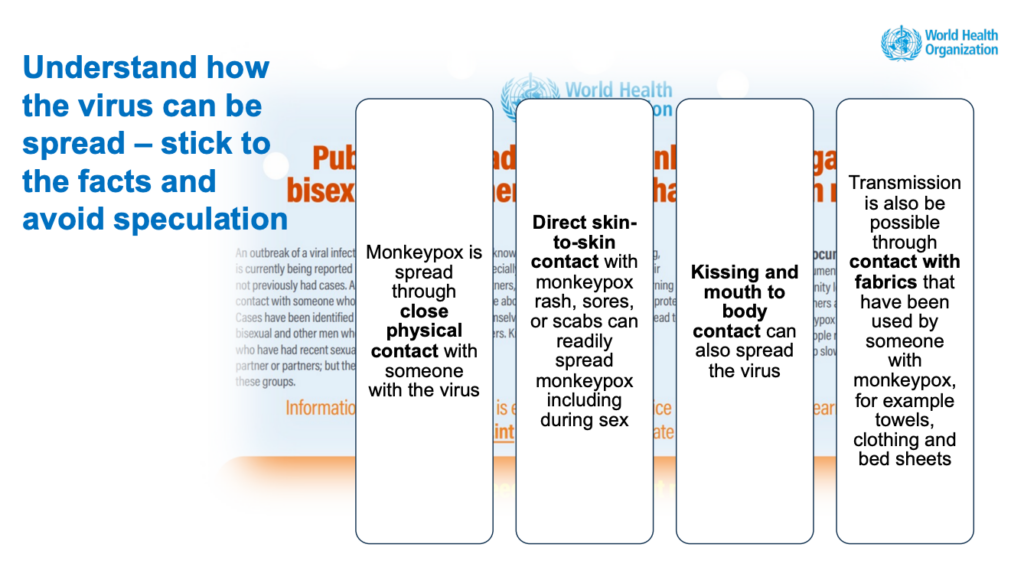
Slide on monkeypox transmission from a July 2022 webinar presentation by Andrew Seale, a World Health Organization advisor. Image: WHO
Research Roundup
“Epidemiologic and Clinical Characteristics of Monkeypox Cases — United States, May 17–July 22, 2022”
David Philpott; et al. CDC’s Morbidity and Mortality Weekly Report, August 2022.
The report describes the characteristics of 1,195 human monkeypox case reports in the US between May 17, when the first US case related to the 2022 outbreak was identified, and July 22. Of those, 99% were men and 94% reported male-to-male sexual or intimate contact during the three weeks before symptoms began. About 41% were white, 28% were Hispanic or Latino, 26% were Black and 5% Asian. Genital rash, although reported in fewer than half of cases, was common; 36% of persons developed rash in four or more body regions, the authors report. About 41% of patients were living with HIV.
“A substantial proportion of monkeypox cases have been reported among persons with HIV infection, and efforts are underway to characterize monkeypox clinical outcomes among these persons,” the authors wrote. “Clinicians and health officials implementing monkeypox education, testing, and prevention efforts should also incorporate recommended interventions for other conditions occurring among gay and bisexual men, including HIV infection, sexually transmitted infections, substance use, and viral hepatitis.”
“Epidemiology of Early Monkeypox Virus Transmission in Sexual Networks of Gay and Bisexual Men, England, 2022”
Amoolya Vusirikala; et al. CDC’s Emerging Infectious Diseases Journal, August 2022.
Published by researchers at the UK Health Security Agency in London, the study is based on phone interviews with 45 patients with monkeypox and was conducted between May 25 and 30, 2022. All but one person identified as gay or bisexual. About a quarter reported living with HIV and were receiving treatment. Sixty-four percent of patients reported attending sex-on-premises venues, such as bathhouses, or festivals, private sex parties or cruising grounds, in the three weeks before developing symptoms. The authors defined cruising as sexual activity with anonymous people in public spaces. However, 36% didn’t report any of those activities. Instead, they had had sexual activity with new partners or had met via dating apps.
“Our findings suggest that sustained domestic MPXV [monkeypox virus] transmission in sexual networks of GBMSM [gay, bisexual men, and men who have sex with men] in England has been occurring since at least April 2022, with potential importations and exportations from other countries in Europe,” the authors wrote. “To achieve outbreak control, targeted interventions for venues and their users are vital, including supporting enhanced cleaning of venues to prevent transmission via fomites, targeted health promotion to build awareness and inform risk management, and innovative approaches to support contact tracing of venue attendees.”
Two related studies: “Demographic and Clinical Characteristics of Confirmed Human Monkeypox Virus Cases in Individuals Attending a Sexual Health Centre in London, UK: An Observational Analysis,” by Nicolò Girometti; et al., published in The Lancet Infectious Diseases in July 2022. And “Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series,” by Aatish Patel; et al., published in the British Medical Journal in July 2022.
“Tecovirimat and the Treatment of Monkeypox — Past, Present, and Future Considerations”
Drs. Adam Sherwat, John Brooks, Debra Birnkrant and Peter Kim. NEJM, August 2022.
The perspective article discusses the nuances in use of antiviral drug tecovirimat (TPOXX), which has been approved for the treatment of smallpox under a regulation known as the “Animal Rule” and raises a conundrum: “How to manage compassionate access to a drug whose safety and efficacy in humans have not been established.”
“Technical Report: Multi-National Monkeypox Outbreak, United States, 2022”
US Centers for Disease Control and Prevention, July 2022.
The report provided an overview of monkeypox cases in the US as of July 25, 2022, including 3,487 cases in 45 states, the District of Columbia and Puerto Rico. The median patient age was 35. Of the 1,383 patients with information on sex assigned at birth, 99% were men. Of the 624 with information on sexual activity, 99% reported male-to-male sexual contact. Race and ethnicity data were missing for a large number of cases, but the available information showed that 38% were white, 32% were Hispanic, and 26% were Black.
Many of the initial patients reported international travel in the 21 days before symptoms appears, visiting countries where monkeypox was not endemic. Many reported participating in large festivals and other activities where close, personal, skin-to-skin contact likely occurred.
The technical report listed several priority research questions, including what medical interventions can be effective, how the virus is transmitted and how best to monitor mis- and disinformation and counter them.
“Frequent Detection of Monkeypox Virus DNA in Saliva, Semen, and Other Clinical Samples from 12 Patients, Barcelona, Spain, May to June 2022”
Aida Peiró-Mestres; et al. Eurosurveillance, July 2022.
Analysis of 147 clinical samples collected at different times from 12 patients revealed that the monkeypox virus was present in saliva from all cases. It was also frequently present in rectal swab, nose swabs, semen, urine, and feces.
“Our results contribute to an improved understanding of a likely complex transmission puzzle and underline other immediate areas for research such as the infectivity of bodily fluids, the frequency of secondary and asymptomatic cases or the impact of social and behavioral factors affecting viral transmission,” the authors wrote.
“The Changing Epidemiology of Human Monkeypox — A Potential Threat? A Systematic Review”
Eveline Bunge; et al. PLOS Neglected Tropical Diseases, February 2022.
Published shortly before the current outbreak, this systematic review of existing literature was one of several papers sounding the alarm about the public health implications of the international community ignoring monkeypox.
“The waning population immunity associated with discontinuation of smallpox vaccination has established the landscape for the resurgence of monkeypox,” the authors wrote. “In light of the current environment for pandemic threats, the public health importance of monkeypox disease should not be underestimated. International support for increased surveillance and detection of monkeypox cases are essential tools for understanding the continuously changing epidemiology of this resurging disease.”
“Human Monkeypox — After 40 Years, An Unintended Consequence of Smallpox Eradication”
Karl Simpson; et al. Vaccine, July 2020.
The report noted that since the eradication of smallpox in 1980, about 70% of the world’s population is no longer protected against smallpox and that monkeypox, which is from the same family of viruses, is now a re-emerging disease.
“Monkeypox has been viewed as ‘just another neglected disease.’ Global travel and easy access to remote and potentially monkeypox-endemic regions are a cause for increasing global vigilance,” the authors wrote. “As monkeypox is no longer a rare disease, there is need for more rigorous epidemiological studies, with particular reference to zoonotic hosts, transmission potential and human case severity.”
“Human Monkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention”
Dr. Eskild Petersen; et al., Infectious Disease Clinics of North America, December 2019.
The study provided an overview of monkeypox and related outbreaks over the decades and stresses that monkeypox is “no longer ‘a rare viral zoonotic disease that occurs primarily in remote parts of Central and West Africa, near tropical rainforests.’”
“A Systematic Review of the Epidemiology of Human Monkeypox Outbreaks and Implications for Outbreak Strategy”
Ellen Beer and V. Bhargavi Rao. PLOS Neglected Tropical Diseases, October 2019.
The report reviewed 71 documents, including situation reports, investigations, and case reports published between 1972 and 2018. The study provides a detailed analysis of available data.
The authors noted that few studies based on virus samples were available. “Overall, samples are seldom taken, and very few cases are laboratory-confirmed,” they wrote. “Significant improvements in the quality and quantity of outbreak data collection are urgently needed to improve the monkeypox research portfolio to inform appropriate case management and public health response.”
“The 2017 human monkeypox outbreak in Nigeria — Report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria”
Dimie Ogoina; et al. PLOS One, April 2019.
The study investigated the 2017 monkeypox outbreak in Nigeria. While Nigeria reported three monkeypox cases between 1970 and 2017, it had a large outbreak with 228 suspected cases in 2017. Researchers reviewed clinical characteristics of 21 cases at Niger Delta University Teaching Hospital, between September and December 2017. The median age was 29, ranging from 6 to 45 years. About 80% were male.
Most patients expressed fear and anxiety over facing stigma and discrimination from hospital staff, members of the community and family members, the authors wrote.
The most prominent challenge in hospital response was delay in testing because none of the labs in Nigeria could test for the infection when the outbreak began.
“The Nigeria outbreak was characterized by predominant infection among young adult males and significant person-to-person secondary transmission,” the authors wrote. “These findings differ from previous reports … of human monkeypox where children below 10 years of age comprised 83% of the cases and secondary transmission was observed to be rare.”
The authors defined secondary transmission as person-to-person transmission via respiratory droplets, direct contact with infected secretions of patients, or from contact with contaminated patient environment, like bedding.
The authors also noted that a substantial number of young adults had genital ulcers, which was less common in previously reported cases. “The role of genital secretions in transmission of human monkeypox, however deserves further studies,” they wrote.
“Extended Human-to-Human Transmission during a Monkeypox Outbreak in the Democratic Republic of the Congo”
Leisha Diane Nolen; et al. CDC’s Emerging Infectious Diseases Journal, June 2016.
The study reported a notable increase in monkeypox cases in the Democratic Republic of Congo, where the infection is endemic. The report included 104 suspected cases between July and December 2013, compared with 13 cases in 2012 and 17 cases in 2011. In 50% of the cases, the virus was spread among the people in the household. The median age of patients was 10 with an age range between 4 months and 68 years. About 57% were male. There were 10 deaths. The infections were likely caused by exposure to wild animals or an infected individual.
“The high attack rate and transmission observed in this study reinforce the importance of surveillance and rapid identification of monkeypox cases,” the authors wrote. “Community education and training are needed to prevent transmission of MPXV infection during outbreaks.”
More Recommended Reading
- What You Need to Know About the History of Monkeypox, by Simar Bajaj, published in the Smithsonian Magazine in June 2022, delved into the history of monkeypox.
- What Scientists Know — and Don’t Know — About How Monkeypox Spreads, by Megan Molteni, published in STAT in August 2022, explained in detail what’s known and unknown about the routes of virus transmission. “What’s clear from the epidemiological evidence so far is that the current monkeypox epidemic is being driven overwhelmingly by the first of these [direct skin-to-skin contact] — in particular, close intimate contact between sexual partners,” she wrote.
- Why the Monkeypox Outbreak is Mostly Affecting Men Who Have Sex with Men, by Kai Kupferschmidt, published in Science Magazine in June 2022, explained how interconnected sexual networks within the community of men who have sex with men may give the virus the ability to spread in ways that it can’t in the general population.
- He Discovered the Origin of the Monkeypox Outbreak — and Tried to Warn the World, by Michaeleen Doucleff for NPR, published in July 2022, told the story of Dr. Dimie Ogoina, who diagnosed the first known case of the current international monkeypox outbreak in an 11 year-old-boy in 2017.
- How is Monkeypox Spread? is a good explainer published in August 2022 by epidemiologist Katelyn Jetelina in her Substack.
- Fighting Monkeypox, Sexual Health Clinics Are Underfunded and Ill-Equipped, by Liz Szabo and Lauren Weber for Kaiser Health News, published in July 2022, noted: “Sexual health clinics have been stretched so thin that many lack the staff to perform such basic duties as contacting and treating the partners of infected patients.”
- New Data From Several States Show Racial Disparities in Monkeypox Infections, by Usha Lee McFarling, Katherine Gilyard, and Akila Muthukumar, published in STAT in August 2022, highlighted extreme racial disparities in monkeypox cases in some states, compounded by lack of access to vaccine.
- What Does It Mean to Declare Monkeypox a PHEIC? by Talha Burki, published in Lancet Infectious Diseases in August 2020, explained what a public health emergency declaration by WHO does and doesn’t do. In another article, Monkeypox as a PHEIC: Implications for Global Health Governance, published in August 2022 in The Lancet, Clare Wenham and Mark Eccleston-Turner also explored the implications of the declaration.
Resources for Journalists
- Several journals, including JAMA, Nature journals, BMC journals and Annals of Internal Medicine have been providing free public access to their monkeypox content.
- You can find WHO’s main page for monkeypox here and the CDC’s here.
- WHO has weekly reports on emergency situations updates for monkeypox.
- CDC’s “2022 Monkeypox Outbreak Global Map” keeps track of confirmed cases and deaths. WHO also keeps track of reported cases on its Health Emergency Dashboard. Our World in Data is another source for numbers and reports seven-day averages and weekly trends.
- Johns Hopkins University’s Center for Health Security has a weekly outbreak alert for monkeypox and provides a comprehensive overview of the latest developments and research in the US and around the world.
- Special Advisory: Covering Monkeypox by the Association of LGTBQ Journalists provides guidance to journalists and newsrooms on the language they use when covering monkeypox. How to Talk About Monkeypox Effectively, Without Stigmatizing Gay Men, published on NPR’s All Things Considered in August 2022, is also a good guide. And CNN’s Sara Ashley O’Brien has sage advice about choosing images for your monkeypox stories.
- Reducing Stigma in Monkeypox Communication and Community Engagement, a document by the CDC, discusses how the agency is framing communication around monkeypox to avoid marginalizing stigmatizing groups that may be at increased risk of the infection.
- How to Cover Health Inequities in US Monkeypox Data Trends, by Margarita Birnbaum and Bara Vaida, published on Association of Health Care Journalists’ blog Covering Health in August 2022, is a tip sheet to help journalists shed light on the disparities in monkeypox infections.
- FDA Monkeypox Response explains the role of FDA in the current public health emergency.
- If you’re curious about monkeypox strains, check Nextstrain, an open source project that provides a view of publicly-available data along visualizations for use by anyone.
- In Monkeypox Experts to Follow on Social Media, also published on the Covering Health blog, Bara Vaida shares her Twitter list of monkeypox experts.

Slide on avoiding monkeypox stigma from a July 2022 webinar presentation by Andrew Seale, a World Health Organization advisor. Image: WHO
Free Multimedia Resources for News Stories
- The CDC has these graphics, images and videos about monkeypox. It also has b-roll of the agency’s buildings.
- WHO has a large collection of photos, including people getting vaccinated and patients with monkeypox.
- This WHO graphic on recovering from monkeypox at home shows what steps individuals should take.
- SciLine, a free service for journalists based at the American Association for Advancement of Science, has several video clips of expert interviews, which you can embed in your stories.
This post was originally published on The Journalist’s Resource. It is reprinted here using Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license.
Additional Resources
GIJN Health and Medicine Reporting Guide
How Reporters Can Flatten the Stress Curve While Covering the Pandemic
Medical, Digital, and Legal Safety Tips for Journalists Covering the Pandemic
 Naseem Miller joined The Journalist’s Resource in 2021 after working as a health reporter in local newspapers and national medical trade publications for nearly two decades. She covers health and medicine with a focus on disparities. She co-started and administers the Journalists Covering Trauma Facebook page and frequently speaks to journalists about trauma and trauma-informed reporting.
Naseem Miller joined The Journalist’s Resource in 2021 after working as a health reporter in local newspapers and national medical trade publications for nearly two decades. She covers health and medicine with a focus on disparities. She co-started and administers the Journalists Covering Trauma Facebook page and frequently speaks to journalists about trauma and trauma-informed reporting.