Image: Courtesy of TBIJ
From the Hospital to the Lab: How We Reported the Snakebite Scandal
Imagine that every time you go to work, you’re put at risk of a disease that could kill you in 30 minutes. What if the only medicine that can save you isn’t available in the first or second hospital you visit? And when you do track it down, it doesn’t even work.
That’s the stark reality faced by rural workers across sub-Saharan Africa, something my editor Fiona and I were growing to understand as we trawled along the coast of Kenya last year on a reporting trip. The disease we were looking into? Venomous snakebite.
First, we needed to learn the basics. And the person everyone said we needed to talk to was Eugene Erulu, a doctor with decades of experience treating snakebite. He was a hard man to pin down and it took the best part of two days — plus several hours staring at the ceiling in his waiting room — to get a word with him. But once he started speaking, his expertise was obvious.
“It was devastating because the patients never got the correct antivenom,” he told me in his office at Watamu Hospital, Kilifi County. He was describing repeated cases where the available antivenoms had been, in his opinion, useless. He named specific manufacturers whose drugs he refused to use.
We were especially struck by Erulu’s frankness. Most other people we’d spoken to on the subject had carefully evaded questions or agreed to speak only off the record. But Erulu didn’t flinch.
He was adamant that companies had made bad antivenom and was clear on the damage done. “Patients have died. Patients have lost limbs,” he said.
It’s people like Erulu that get an investigation off the ground.
You might think of snakebites as a niche issue rather than a devastating one. But it is thought to kill somewhere between 80,000 and 140,000 people a year. And travelling from clinic to clinic, we saw a trail of harm comparable to major diseases that result in far more media coverage — and much more money.
A short drive up the coast in Malindi, a sunny beach town adored by Italian tourists, we visited a bustling referral hospital. A solemn farmworker called Safari Charo Ndindow was nursing a heavily bandaged arm, having been bitten by a cobra a few days before. He had travelled to three clinics before receiving treatment, then had to be transferred to a fourth, blacking out on the way. Antivenom was hard to find wherever we went. It felt like people were hardly being given a fighting chance.
Ndindow was unable to work and worried what that would mean for his family. Those bitten are often the breadwinners, people who spend their days out herding cattle or tilling the land. Like many diseases, those most severely affected by snakebite have the fewest resources to deal with its consequences. We heard of people selling everything they had for a single vial of antivenom — and with no guarantee that it would work.

Charo Ndindow sits in a hospital. One year after being bitten by a cobra and treated with antivenom, he doesn't have use of his left hand. Image: Courtesy of TBIJ
An obvious question emerged. How had this situation been allowed to persist?
“I always say, if you had politicians or tourists getting bitten, the government would have to take a little bit more interest and the solution might come a lot quicker,” said Kyle Ray, when we visited him at the Watamu Snake Farm education centre. “But it’s the poor guys who don’t have a voice who are affected.”
As Fiona and I headed back to the UK, it seemed we had all the ingredients of a huge story. A threat to human life, bad actors, systemic failures, and gross injustice. And we knew by this point that the issues we’d seen first-hand stretched across sub-Saharan Africa.
We now needed to find out all about the manufacturers, patients, regulations, and existing research. So along with our colleagues, we pored over shipping data and leaked emails; we spoke to people from 25 countries, including frontline doctors, scientists, antivenom manufacturers, and charity workers (one of whom told me she’d put a black mamba in my bed if I misused the information she gave me).
The message we kept hearing was clear: some antivenoms were not working. The hard part was getting irrefutable scientific evidence. So we contacted Professor Juan Calvete of the Instituto de Biomedicina de Valencia, the WHO’s go-to expert for testing antivenoms. We needed a way to measure a manufacturer’s claims about its medicine against the reality of its actual effects.
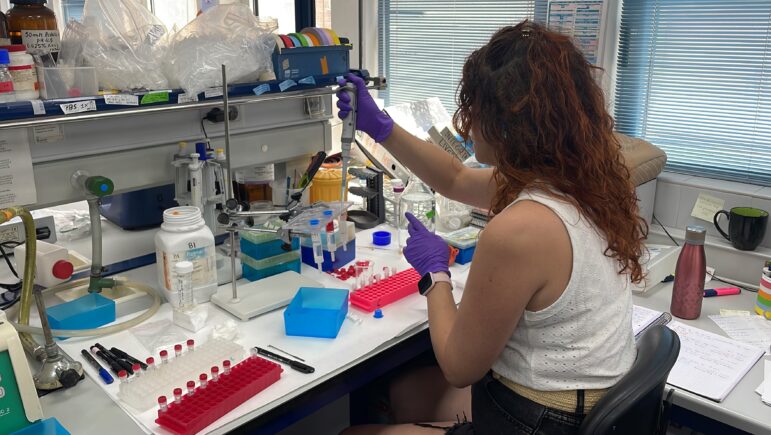
TBIJ tested numerous antivenoms to gauge their efficacy — or lack thereof. Image: Courtesy of TBIJ
Calvete’s testing did just that. And once we unpacked the results — with the extensive input of yet more experts — the findings were astounding. Some antivenoms, for instance, could require more than 70 vials to effectively treat some bites. We had our story.
It was almost a year from that chat in Erulu’s office to the story getting published. But publication isn’t the end of the road. Since the story came out, we have taken our findings to national regulators, the World Health Organization, drug manufacturers, their parent companies and even a Bollywood celebrity ambassador.
The hope now is that those in power will finally start paying attention to this most neglected of tropical diseases — rather than looking the other way as thousands continue to die.
Editor's Note: This story was originally published by The Bureau of Investigative Journalism and is republished here with permission.
 Paul Eccles is a reporter and impact producer on TBIJ’s Global Health team. Since joining TBIJ, he has worked on investigations into access to oxygen, vaccine inequality, digital advertising and Big Tobacco.
Paul Eccles is a reporter and impact producer on TBIJ’s Global Health team. Since joining TBIJ, he has worked on investigations into access to oxygen, vaccine inequality, digital advertising and Big Tobacco.
 Fiona Walker is an award-winning journalist, documentary-maker and podcaster. As an investigative journalist, she has reported for Panorama and BBC Scotland Investigates, exposing abuse and uncovering fraud. She is driven by injustice and, during her career, has often focused on health – with her time as a BBC health correspondent spanning the Covid-19 pandemic. Her podcast, The Doorstep Murder, reached number one in the iTunes UK podcast charts and was nominated for a British Podcast Award. Fiona worked at the BBC for 22 years.
Fiona Walker is an award-winning journalist, documentary-maker and podcaster. As an investigative journalist, she has reported for Panorama and BBC Scotland Investigates, exposing abuse and uncovering fraud. She is driven by injustice and, during her career, has often focused on health – with her time as a BBC health correspondent spanning the Covid-19 pandemic. Her podcast, The Doorstep Murder, reached number one in the iTunes UK podcast charts and was nominated for a British Podcast Award. Fiona worked at the BBC for 22 years.